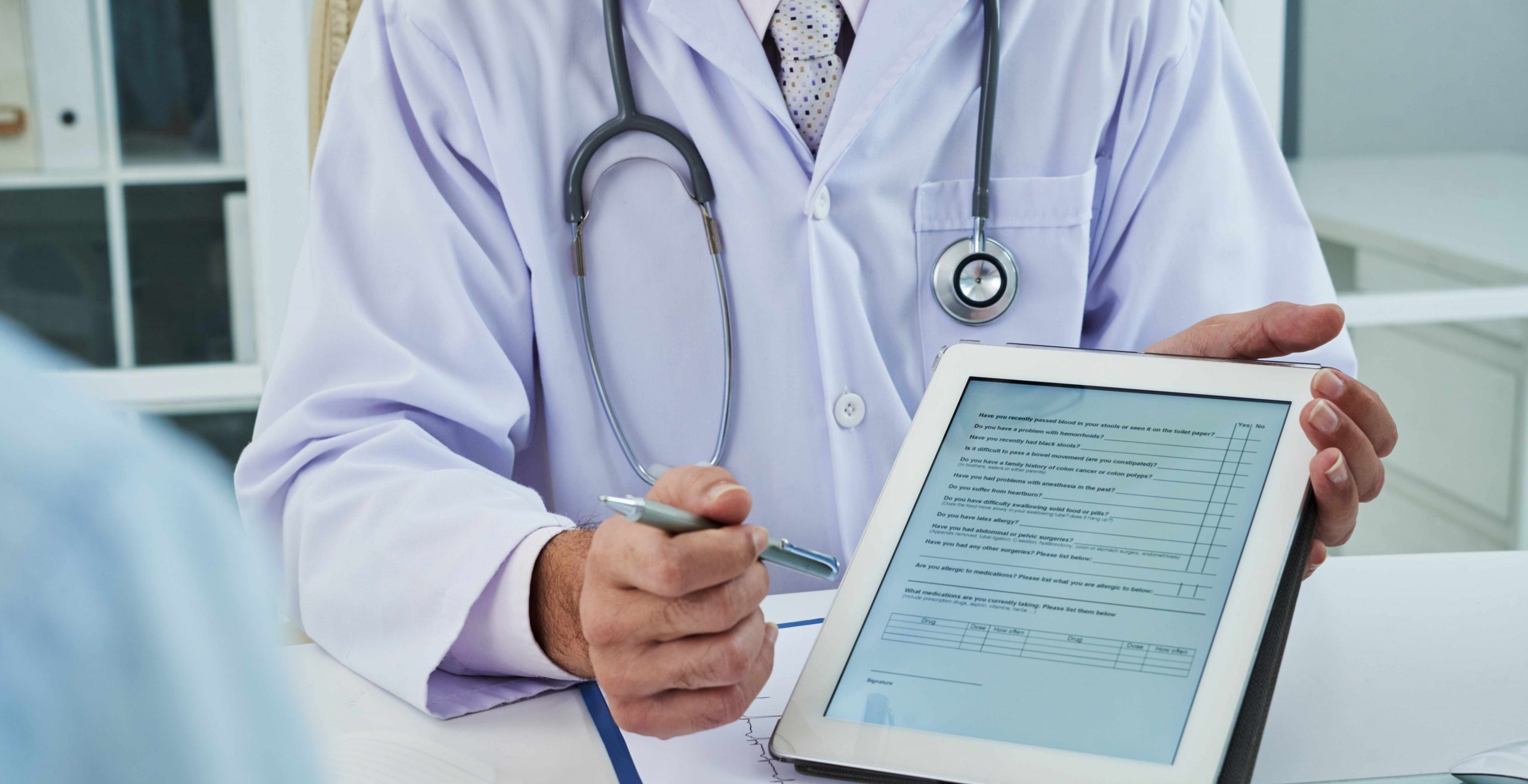
Revenue cycle management (RCM) is a process that manages claims processing, payment, and revenue generation. It entails using technology to keep track of the claims process at every stage, so that the healthcare provider doing the billing can follow the process, address any issues, and allow a steady stream of revenue.
Payments that are denied can mean your company could lose up to 90% in revenue. Having RCM in place ensures that payments are made.
RCM encompasses everything from determining patient insurance eligibility, collecting co-pays to properly code claims using ICD-10. Time management and efficiency play pivotal roles in RCM, and a physician’s or hospital’s choice of an EMR will largely depend on how their RCM is implemented.